The second stage of labour
In this article:
- Progression of labour
- What is the second stage of labour and when does it begin?
- The journey through the birth canal
- How long does the second stage of labour last?
- What will I feel during the second stage?
- What are the best positions for pushing?
- Methods to help with the second stage of labour
- Complications
- When will doctors get involved?
- Twin pregnancies
- Main points

Progression of labour
After nine months of pregnancy and the first stage of labour, you will finally reach the second stage of labour when your cervix is 10cm dilated and the baby is ready to be born.
What is the second stage of labour and when does it begin?
The second stage of labour starts from the time that your cervix is fully dilated (10cm open) until your baby has been delivered. The second stage of labour can also be divided into the passive stage (propulsive) and the active stage (expulsive). The passive stage occurs when the cervix is fully dilated but active pushing is not commenced. This may be because the baby’s head is still high in the pelvis and your body has no urge to push or it may be because an epidural is being used for pain relief. Usually more time will be allowed to let the baby’s head descend further into the pelvis from the power of the uterine contractions alone.
The active stage is when you start pushing. This may be immediately after full dilation of the cervix if you have a strong urge to push or the baby’s head is already very low in the birth canal. For some women there is no distinction between the passive and active stages because the urge to push may be very strong or involuntary immediately after full dilatation.
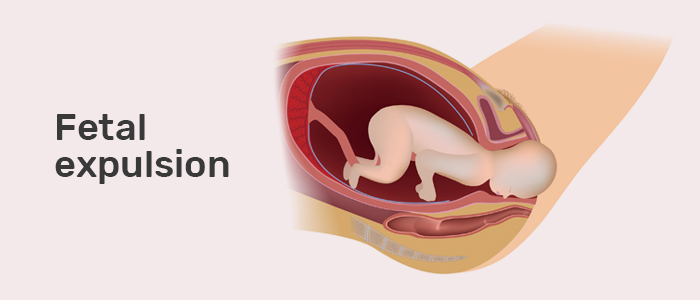
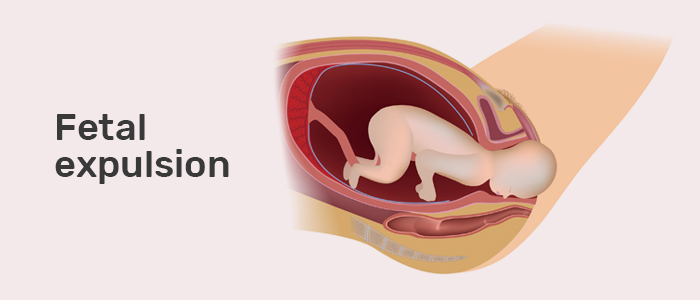
The journey through the birth canal
The birth canal is made up of the pelvic bones around the sides and the pelvic floor muscles at the bottom (a hammock of muscles at the bottom of the pelvis). During childbirth, the baby’s head will enter the pelvis sideways (occipito-transverse or OT position) as the pelvis is wider than it is deep at this point. With contractions, the baby is moved down the birth canal where it narrows and the head rotates by 90° into a forward-backward position with the chin tucked onto the baby’s chest (flexion). For most women the baby will turn to face the mum’s back (occipito-anterior or OA position). This is beneficial for labour as this is the smallest presenting diameter of the baby’s head and therefore makes delivery easier. Occasionally babies rotate so that they end up back-to-back with mum or “star-gazing” (occipito-posterior or OP position). This is a slightly larger presenting diameter and so in any such instance the second stage may be longer or may require medical assistance. When the head reaches the pelvic floor it is likely you will then experience strong urges to push.
How long does the second stage of labour last?
Overall, the second stage can last from just a few minutes to as long as a few hours. Certain factors influence the length of the second stage — for example, women who have had a baby before may have a shorter second stage than first-time mums, and women who have an epidural for pain relief may have a longer second stage.
NICE (The National Institute Clinical Excellence) provides guidance on how long the second stage of labour should last depending on a woman’s individual circumstances. If you are in labour with your first baby, birth would be expected to take place within three hours of the start of the active (expulsive) stage. If you have previously had a baby via vaginal delivery, birth is expected to take place within two hours from the start of the active second stage. If you have had a previous baby delivered by caesarean section the guidance would be to limit the active phase of pushing to one hour to avoid strain on the old scar on the womb. If an epidural is being used for pain relief your healthcare practitioner may advise a longer passive stage to allow the power of the uterine contractions to assist with both descent and rotation of your baby’s head prior to active pushing.
Pushing too early and sustained bearing down can be associated with complications for mum and baby. Research has shown that delaying active pushing until you have an urge to push or the baby’s head is visible reduces the incidence of forceps delivery and caesarean section; delaying pushing is also likely to shorten the most exhausting part of labour.
What will I feel during the second stage?
Everyone is different and the experience of the second stage can vary dramatically based on the type of pain relief used, the position and size of the baby and how quickly the labour has progressed up until this point.
Generally, the frequency and duration of the contractions (how often they come and how long they last) remains the same as the first stage of labour but the intensity or strength may change. If the contractions decrease or stop at the second stage, this can be a sign of potential complications (see below) and will need a review from an obstetrician. When the baby’s head is very low in the pelvis and reaching the pelvic floor, you might feel a strong pressure (some women describe it as a similar feeling to needing to open their bowels). Lots of women report relief from contractions as they start pushing with their contractions.
For women with an epidural, the perception of contractions should not change in the second stage. For some there won’t be any feeling at all. If this is the case, then the midwife will feel your bump for the contractions and let you know when it is time to push. Epidurals are often not able to take away the pressure sensation when the baby reaches the pelvic floor so even if a woman has had an epidural she may still feel this final stage of labour, though it is not likely to be as painful and the experience of sensation may actually help with direct pushing.
As the baby’s head is being delivered (crowning), there is a stretching sensation of the vaginal skin that some women describe as a burning feeling. Usually this stage of labour is very short and easily forgotten as your new baby is delivered. If an episiotomy is needed at this stage to prevent tearing, local anaesthetic is given to numb the area and you shouldn’t feel anything at all.
What are the best positions for pushing?
The position you take is really up to you and you will be encouraged to follow your body’s urges and push in whichever position you feel comfortable. It is discouraged generally and also by NICE, however, to lie on your back or recline significantly (semi-recumbent position) when you are pushing. Using gravity to aid your body’s active pushing is assisted by being upright. This can be achieved by sitting up, squatting, being in the all fours position or standing or leaning on the delivery bed. Modern birthing beds can be modified to aid your upright position. The use of birthing balls and various labour swings and seats (dependent on access by your local maternity unit) can also aid you in finding the most comfortable position. If you are using an epidural for pain relief this will limit you to certain positions; however with the use of modern birthing beds an upright pushing position is achievable.
Methods to help with the second stage of labour
Having a supportive birth partner has been shown to reduce the need for instrumental deliveries and caesarean sections. One-to-one care alongside a birthing partner allows your emotional, physical and psychological needs to be met. Maintaining adequate hydration and good pain relief are also shown to reduce instrumental rates.
Complications
Contractions are stressful for babies but they are designed to be able to tolerate them as usually there is a rest period of at least a minute between each contraction. However, at any point during labour, a baby may not tolerate the contractions. This might be due to the position of the baby and the umbilical cord (not serious and usually resolves) or because the baby is not getting enough oxygen during the contractions (more serious and will need review from a doctor). The chance of the baby becoming distressed is often higher in the second stage as there are contractions as well as pushing.
Distress is detected as changes in the baby’s heart rate pattern and will alert midwives and doctors to any problems. If there are significant concerns, then delivery may be expedited by an instrumental delivery or a caesarean section (if the head is very high or not in position to be delivered with an instrument).
Sometimes, even when the cervix is fully dilated, the baby will not descend all the way through the birth canal, and this may be the case even with perfect contractions and pushing. This is known as lack of progress and may be accompanied with a reduction in the frequency of your contractions. It might be that the baby is too large for the pelvis (true cephalo-pelvic disproportion) or the baby is in a difficult position — e.g. OP position or back-to-back. Sometimes a midwife or doctor may be able to gently encourage the head into a more favourable OA position. If there is lack of progress, a doctor will evaluate the position of the baby and how low it is (station) to see whether it can be delivered vaginally. Sometimes it may not be safe to continue with natural childbirth and a caesarean section may be offered at this stage as the safest way to deliver your baby.
A less common complication can occur once your baby’s head has been delivered. This is called shoulder dystocia and is when the baby’s shoulders get stuck against your pelvic bones. This complication requires emergency attention and in the majority of cases is resolved with a change in the mother’s position.
Up to 90% of women will have some form of vaginal tearing and this is not considered a complication but a natural part of childbirth. Most of the time it is mild and may not even require stitches. More rarely a deeper tear can occur that involves the muscles (2nd degree tear) or the anal sphincter (3rd and 4th degree tears). This requires careful repair. See more on perineal tears.
When will doctors get involved?
If at any time during the second stage of labour there is slow progress or any suspicion that your baby is becoming distressed a medical review will be required. If your baby’s heart rate has been listened to only after every contraction you may be put on a continuous heart rate monitor (CTG) to obtain a clearer picture of how your baby is coping with the second stage of labour. A doctor may examine you vaginally to access the position of baby’s head and to determine how well your contractions are moving it down the birth canal. If there are any concerns a doctor may wish to expedite the delivery by offering an instrumental delivery (forceps or ventouse) or more rarely, a caesarean section.
Twin pregnancies
The principles are the same as for a singleton pregnancy: have regular strong contractions, monitor the baby (both in this case) for signs of distress and ensure good progress through the birth canal.
In twin pregnancies it can be difficult to monitor both baby’s heart rates separately as they are so close together in the womb. To be certain both babies are monitored separately, a small clip (fetal scalp electrode or FSE) can be applied to the first twin’s head in the vagina and the second twin monitored via standard abdominal monitoring. If there are clear and separate heart rates for both twins using abdominal monitors, an FSE may not be needed.
The delivery of the first twin is no different from when there is a single baby being delivered. The second twin is the higher risk delivery as it may be breech or, if head-down, it can rotate into a transverse or breech position as there will be a lot of room in the womb after their sibling has exited. To avoid this a healthcare practitioner will usually try to stabilise the second twin by applying pressure to your abdomen and a scan may be done to check their position. Sometimes the contractions stop or slow down after the first baby is delivered and a hormone drip (oxytocin) may be needed to keep them going for delivery of the second baby. Ideally there should be no more than thirty minutes delay between delivery of both babies.
There will usually be more people in the room if you are having twins (to ensure both babies are attended to!) and often twins are delivered in the operating theatre as it is a large space and the ideal place to be if any complications arise.
Main points
The second stage starts when the cervix is fully dilated and ends with the delivery of the baby.
- Pushing may not start straight away in the second stage if the baby’s head is still high in the birth canal or an epidural is being used for pain relief (passive second stage).
- The pushing part of the second stage (active stage) should not last more than three hours in first-time mums or two hours if the woman has previously had another baby, though often it is a lot shorter.
- Babies enter the pelvis in a sideways position and rotate by 90° so that they face the mother’s back or, less commonly, a back-to-back “star-gazing position”.
- The second stage of labour may feel more intense and women may experience more pressure as the baby’s head is on the pelvic floor. If an epidural is being used, there may be no sensation at all, although in some cases there may still be some sensation of pressure.
- Pushing is encouraged in whichever position feels comfortable to you, though it is best to let gravity help and to avoid lying on your back.
- Having a supportive birthing partner can reduce the length of labour and the need for any medical intervention.
- Babies can become distressed during the second stage of labour or may fail to descend through the birth canal. Both situations warrant a review from an obstetrician.
- The delivery of the second twin in twin pregnancies is higher risk and requires more people to be present.
References
NICE: Intrapartum care for healthy women and babies Clinical guideline [CG190] Published date: 03 December 2014 Last updated: 21 February 2017
RCOG: eLearing Management of normal Labour and Birth, Felicity Watson (2020).
More articles from this expert
Important – If you or your child are unwell you should seek medical advice from a professional – contact your GP or visit an A&E department in an emergency. While My BabyManual strives to provide dependable and trusted information on pregnancy and childcare 24/7 via our website pages, we cannot provide individual answers to specific healthcare questions.



